In the realm of healthcare policy, one term that often arises is “Certificate-of-Need” (CON). This regulatory framework aims to govern the establishment or expansion of healthcare facilities and services. In this blog post, we’ll dive into the concept of Certificate-of-Need, explore its historical background, and examine the pros and cons.
What is a Certificate-of-Need?
A Certificate-of-Need is a legal document issued by a state or regional regulatory body that grants permission to healthcare providers to initiate new medical facilities, expand existing ones, or introduce certain medical services or technologies within a defined geographic area. The primary objective of CON laws is to control healthcare costs, prevent unnecessary duplication of services, and maintain quality care standards.
The History of Certificate-of-Need Legislation
The roots of Certificate-of-Need legislation can be traced back to the 1960s when concerns regarding escalating healthcare costs and surplus healthcare facilities emerged. To address these issues, several states in the United States began implementing CON laws. These laws were predominantly introduced to promote planning, coordination, and efficiency in healthcare delivery by controlling the supply of healthcare services.
Current State
Part of the underlying challenge associated with these laws lies in the fact that they are subject to regulation at the state level, thereby resulting in a lack of uniformity and consistency across different jurisdictions, as each state adheres to its own unique set of processes and requirements.
The impact of the law though is pretty clear – in states where there is no Certificate-of-Need like Texas, there are 450+ Medicare-Certified surgery centers and they are thriving. In other states, like in the Northeast, growth is slow, complicated, and a headache. Plus, the Kaiser Family Foundation found states with CON laws had 11% higher healthcare costs than states without those laws.
At a high-level:
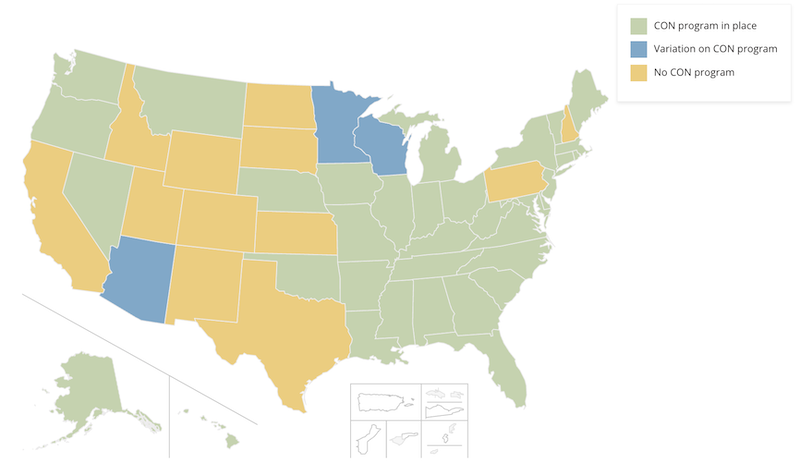
Image Source: NCSL
12 states have no program: California, Idaho, Wyoming, Utah, Colorado, New Mexico, Texas, North Dakota, South Dakota, Kansas, Pennsylvania, New Hampshire
3 states have some variation of a program: Arizona, Minnesota, Wisconsin
35 states have fully intact CON laws: Alabama, Alaska, Arkansas, Connecticut, Delaware, Florida, Georgia, Hawaii, Illinois, Indiana, Iowa, Kentucky, Louisiana, Maine, Maryland, Massachusetts, Michigan, Mississippi, Missouri, Montana, Nebraska, Nevada, New Jersey, New York, North Carolina, Ohio, Oklahoma, Oregon, Rhode Island, South Carolina, Tennessee, Vermont, Virginia, Washington, West Virginia
Things are Changing
The surgery center industry is poised for substantial growth in the upcoming years. The increasing trend of payers urging procedures to outpatient facilities, coupled with the advancements in technology facilitating the performance of more intricate procedures, sets the stage for unprecedented opportunities. However, the frustration arises when the potential expansion is impeded by Certificate-of-Need laws. Despite the substantial investments planned by the top five ASC management groups, these restrictive regulations hinder the industry’s potential for growth.
 According to the NCSL, in 2022, at least 12 states—Arizona, Connecticut, Kentucky, Louisiana, Maryland, Michigan, Mississippi, New York, Ohio, Oklahoma, Vermont and Virginia—and Washington D.C., enacted legislation modifying their CON laws in some capacity.
According to the NCSL, in 2022, at least 12 states—Arizona, Connecticut, Kentucky, Louisiana, Maryland, Michigan, Mississippi, New York, Ohio, Oklahoma, Vermont and Virginia—and Washington D.C., enacted legislation modifying their CON laws in some capacity.
Becker’s ASC Review did a great job of summarizing some of the latest movements and how some management groups are navigating this challenging situation.
It isn’t all bad. Here are the pros:
Cost Control: CON laws are designed to prevent the overinvestment in healthcare infrastructure, which can lead to increased costs. By evaluating the need for new facilities and services, CON laws help avoid unnecessary expenses and promote cost-effective allocation of resources.
Quality Assurance: The regulatory process of obtaining a Certificate-of-Need often involves an assessment of the proposed facility or service’s impact on the existing healthcare landscape. This evaluation ensures that new providers meet certain quality standards, helping to maintain and improve the overall quality of care delivered to patients.
Community Planning: Certificate-of-Need laws encourage systematic and comprehensive healthcare planning. By requiring healthcare providers to demonstrate the need for their proposed services, CON laws facilitate strategic decision-making, prevent excessive competition, and promote the equitable distribution of resources within a community or region.
But, it isn’t all good either. Here are the cons:
Limited Competition & fewer options: Critics argue that CON laws can stifle competition by creating barriers to entry for new providers. The regulatory process and associated costs can deter smaller healthcare providers or entrepreneurs from entering the market, potentially limiting consumer choice and innovation.
Delayed Access to Care: The lengthy and complex process of obtaining a Certificate-of-Need can cause delays in the establishment or expansion of healthcare facilities. These delays may hinder timely access to healthcare services, particularly in areas with a shortage of providers or specialized care.
Inefficiencies and Bureaucracy: Some opponents of CON laws contend that the regulatory process can be burdensome and bureaucratic. The administrative requirements and subjective decision-making involved may introduce inefficiencies, impeding the timely delivery of healthcare services.
They protect established industry leaders from competition by limiting entry into the health care marketplace. Unlike a free-market system, CON laws harm consumers (aka patients), leading to fewer health care options at higher prices. Moreover, CON stifles innovation, leaving patients with less access to emerging technologies in the medical marketplace.
Conclusion
Certificate-of-Need legislation has been a subject of ongoing debate in the healthcare policy arena. While proponents argue that CON laws help control costs, ensure quality care, and promote community planning, opponents raise concerns about limited competition, delayed access to care, and bureaucratic inefficiencies. Striking a balance between these arguments is crucial to ensure an optimal regulatory framework that promotes both affordability and accessibility in healthcare delivery.
Don’t miss out on the good stuff – Subscribe to HST’s Blog & Podcast!
Every month we’ll email you our newest podcast episodes and articles. No fluff – just helpful content delivered right to your inbox.
